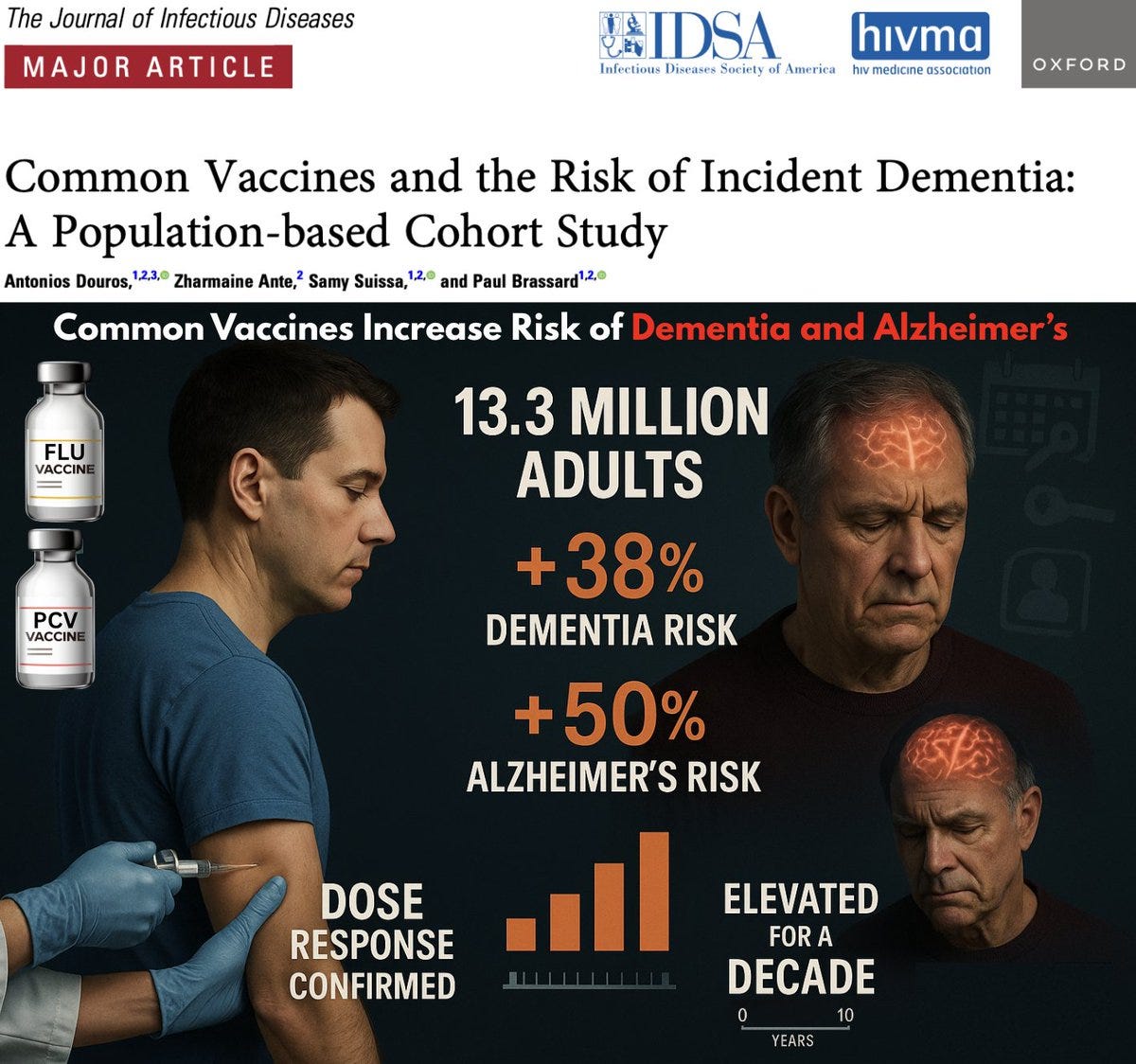
DEMENTIA & ALZHEIMER'S DISEASE CURE PROTOCOL: Study Shows Common Vaccines Increase Risk of Dementia and Alzheimer’s by 38-50%
Not only is there not a single vaccine that is safe, effective or necessary, but all of these medical products are nothing more than highly profitable depopulation injections.
Just as the PSYOP-19 scamdemic exposed the world to the Modified mRNA slow kill bioweapon “vaccine” that not only induces turbo cancer, and other serious adverse events, but also causes prion-based diseases, which are directly responsible for dementia and Alzheimer’s, even in children, so too are all of the other legacy vaccines responsible for this ever-growing neurodegenerative epidemic plaguing all highly vaccinated societies.
And now we have even more irrefutable evidence of just how pernicious all vaccines really are; to wit:
🚨 STUDY: Common Vaccines Increase Risk of Dementia and Alzheimer’s by 38-50%
The single LARGEST vaccine–dementia study ever conducted (n=13.3 million) finds risk intensifies with more doses, remains elevated for a full decade, and is strongest after flu and pneumococcal shots ⬇️📈 38% higher dementia risk after common adult vaccines (OR 1.38)
📈 50% higher Alzheimer’s risk (OR 1.50)
MORE DOSES = MORE DEMENTIA:
1 dose → 📈 OR 1.26
2–3 doses → 📈 OR 1.32
4–7 doses → 📈 OR 1.42
8–12 doses → 📈 OR 1.50
≥13 doses → 📈 OR 1.55
Alzheimer’s dose–response even stronger:
≥4 doses →📈 OR 1.61⏰ Time–response:
Risk peaks at 2–4.9 years after vaccination → 📈 OR 1.56. Risk remains elevated for 10+ years.
💉 Flu shot:
Dementia → 📈 OR 1.39
Alzheimer’s → 📈 OR 1.49
💉 PCV shot:
Dementia/Alzheimer’s → 📈 OR 1.12–1.15
Risks remain elevated even after adjusting for 30+ comorbidities, medications, and applying 10-year lag corrections.
This is one of the strongest, most consistent epidemiologic signals ever published on vaccines and neurodegeneration.
As many longtime readers of this Substack are aware, my mother’s Alzheimer’s was successfully reversed in relatively short order…
…using the following approach:
Dementia & Alzheimer’s Disease Cure Protocol
Fenbendazole 150mg every other day with dinner for 30 days, and repeat every 4 months
Ivermectin 12mg every evening with dinner indefinitely
Low dose lithium orotate 4.8mg capsule in the morning with breakfast and in the evening with dinner indefinitely
VIR-X immune support 2 capsules in the morning with breakfast indefinitely (Quercetin is a critical ingredient in VIR-X, and as per research studies similar to Ivermectin it displayed capabilities against tauopathy by inhibiting the hyperphosphorylation of the tau protein, thus its anti-prion activity helps to reverse Alzheimer’s Disease)
Removal of sugars and carbohydrates, and replacing table sugar with a zero glycemic index, zero calorie, keto friendly rare sugar like FLAV-X
In today’s article we will review just how critical the dietary component of this protocol really is, because if the dementia Alzheimer’s sufferer is consuming a diet high in sugars and carbohydrates (bread, crackers, pasta, rice, potatoes, fruits, tomatoes, candies, ice cream, fruit juices, sodas, processed foods and so on and so forth), then the chances of this protocol successfully restoring cognition are significantly lower.
So, if all of these sugary and high carbohydrate foods are to be avoided, then what is the optimal diet for a demential Alzheimer’s afflicted person?
EGGS
Eating at least one egg per week is associated with a 47% lower risk of developing Alzheimer’s dementia, according to a study published in The Journal of Nutrition.
The study entitled, Association of Egg Intake With Alzheimer’s Dementia Risk in Older Adults: The Rush Memory and Aging Project, found that the association between egg consumption and the risk of Alzheimer’s dementia in older adults was notably reduced.
The researchers analyzed data from 1,024 participants in the Rush Memory and Aging Project, with a mean age of 81.38 years.
Over a mean follow-up period of 6.7 years, they found that consuming more than one egg per week was associated with a 47% lower risk of developing Alzheimer’s dementia compared to those who ate less.
The study, conducted as part of the Rush Memory and Aging Project, revealed the following:
280 participants — 27.3% — were diagnosed with Alzheimer’s dementia.
Participants who consumed more than one egg per week had a 47% lower risk of developing Alzheimer’s dementia compared to those who ate less.
The protective effect was similar for those eating two or more eggs per week.
Analysis of brain autopsies from 578 deceased participants showed that higher egg intake was associated with a lower risk of Alzheimer’s disease pathology in the brain.
Importantly, the researchers found that dietary choline, a nutrient abundant in egg yolks, mediated about 39% of the protective effect against Alzheimer’s dementia.
Eggs also contain omega-3 fatty acids and lutein, two nutrients that have been associated with supporting and protecting brain health.
The study authors concluded:
These findings suggest that frequent egg consumption is associated with a lower risk of Alzheimer’s dementia and AD pathology, and the association with Alzheimer’s dementia is partially mediated through dietary choline.
Eating at least two eggs per day seven days a week would actually be the most effective diet plan to prevent and cure dementia and Alzheimer’s, and that is what my mother does every single morning; in fact, starting one’s day at any age with a quality high fat breakfast ensures brain health, whereas eating bread, oatmeal, and other high carb high sugar meals is ill advised for anyone at risk of any neurodegenerative disease.
HIGH FAT DIET
A high fat diet (HFD) which includes eggs, beef, avocados, nuts, butter, etc. also prevents dementia Alzheimer’s as per a research article entitled, The protective effect of early dietary fat consumption on Alzheimer’s disease–related pathology and cognitive function in mice, which concluded:
The goal of our study was to determine the effect of varied HFD feeding onset on AD-related pathology and cognitive function in Tg6799 AD mice. In this rapid-progression animal model of AD, extracellular plaque deposition begins at 2 months and is readily detectable throughout the cortex and hippocampus by 6 months.15 Furthermore, Tg6799 mice display evidence of spatial memory deficits as early as 4 months of age.15
[…]
In this study, consumption of HFD at an early age led to region-specific as well as widespread reduction of Aβ deposition throughout the brains of AD mice.
[…]
In addition to hallmark AD pathologies, AD is also associated with vascular abnormalities,31, 32 such as parenchymal deposition of fibrinogen, a critical component of the blood coagulation cascade.14, 33-35 Fibrinogen is a glycoprotein found in large quantities in blood.36 In response to injury, fibrinogen is converted to fibrin, the major component of blood clots. Fibrinogen is normally excluded from the brain by the BBB. However, AD patients and mouse models show a loss of BBB integrity,37-41 which promotes fibrinogen extravasation into the brain. We have previously shown that fibrinogen extravasation correlates with the degree of Aβ pathology in AD mice and patients.33, 42-44 Due to its potent pro-inflammatory properties and direct interaction with Aβ,18, 45-47 extravascular fibrinogen may contribute to and/or promote neuroinflammatory responses and neuronal dysfunction.34, 48 In fact, fibrin deposition is present in areas of the brain with prominent synaptic degeneration.33 In this study, we found extravasated fibrinogen in the RSC of 6-month-old AD mice, while their WT littermates showed none.
[…]
In sum, we show that chronic HFD consumption reduced AD-related pathology, including Aβ accumulation, fibrinogen extravasation, and cognitive dysfunction in 6- and 8-month-old AD mice when HFD intake started at or before 3 months of age (before or early-stage disease).
Extrapolating from this study, we may conclude that an HFD with quality whole foods would be beneficial for the prevention and treatment of dementia Alzheimer’s, whereas a low quality HFD of processed foods and products whose ingredients include seed oils will in fact exacerbate dementia and Alzheimer’s; in other words, not all fats are created equally.
MEAT
Previous research studies focused on processed meats as a contributing factor to dementia Alzheimer’s, but just like with lifesaving compounds such as Hydroxychloroquine, these studies were fraudulent by design.
When looking at unadulterated high quality beef that was not processed, the results are radically different, as per a research study entitled, Intake of Meat, Fish, Fruits, and Vegetables and Long-Term Risk of Dementia and Alzheimer’s Disease, which showed the following:
Objective: We aimed to examine the relationship between consumption frequency of meat, fish, fruits, and vegetables and long-term risk of dementia and Alzheimer’s disease (AD), by taking into account this possibility.
Methods: We analyzed data of 5,934 volunteers aged 65 and over from the Three-city study who were followed every 2 to 4 years for 12 years. Dietary habits were assessed at inclusion using a brief food frequency questionnaire. The presence of symptoms of dementia was investigated at each follow-up visit. To limit the risk of protopathic bias, a 4-year lag window between exposure and disease assessment was implemented by excluding from the analyses all dementia cases that occurred during the first four years after inclusion. Analyses were performed using a Cox proportional hazard model and were adjusted for socio-demographic, lifestyle, and health factors.
Results: The average follow-up time was 9.8 years. During this period, 662 cases of dementia, including 466 of AD, were identified. After adjustment, only low meat consumption (≤1 time/week) was associated with an increased risk of dementia and AD compared with regular consumption (≥4 times/week) (HR = 1.58 95% CI = [1.17-2.14], HR = 1.67 95% CI = [1.18-2.37], respectively). No association was found between the consumption of fish, raw fruits, or cooked fruits and vegetables and the risk of dementia or AD.
Conclusion: These findings suggest very low meat consumption increases the long-term risk of dementia and AD, and that a protopathic bias could have impacted finding from previous studies.
Therefore, a higher intake of quality (not processed) meats and fish would be hugely beneficial in reversing Alzheimer’s. In terms of fruits, only low glycemic fruits such as blueberries would be advisable, but all other high glycemic fruits should be avoided, especially fruit juices and apple sauce, etc. & etc.
BLUEBERRIES
The only fruit that would be advisable for dementia Alzheimer’s, with research showing that regular consumption of blueberries aids in reducing the risk of dementia and slowing cognitive decline, particularly in older adults.
Blueberries contain high levels of anthocyanins and other antioxidants, which may protect against oxidative stress, inflammation, and amyloid-beta aggregation—key factors in Alzheimer’s pathology.
Clinical trials have shown that older adults with mild cognitive impairment who consumed blueberry powder or juice demonstrated improved memory, cognitive performance, and brain function compared to placebo groups.
A 2023 pilot study examined the effect of blueberry supplementation on blood-based biomarkers related to Alzheimer’s disease, including amyloid-beta and phosphorylated tau, though no significant changes were reported in this small sample.
While preclinical and epidemiological data are promising, no clinical trials have yet confirmed the effects of blueberries on Alzheimer’s-specific biomarkers in patients with the disease.
As of December 2025, ongoing research continues to explore the preventive potential of blueberries, particularly in at-risk populations such as middle-aged adults with metabolic risk factors.
The research study entitled, Six-month intervention with wild blueberries improved speed of processing in mild cognitive decline: a double-blind, placebo-controlled, randomized clinical trial, concluded the following:
Consumption of wild blueberries for six months improves cognitive aging sequelae by improving the speed of information processing in older adults.
Consuming organic fresh blueberries as well as wild blueberries would be optimal.
FISH
Consuming fish is associated with a lower risk of cognitive impairment, dementia, and Alzheimer’s disease, with a meta-analysis of 35 observational studies showing that individuals with the highest fish consumption had a 18% lower risk of cognitive impairment/decline (RR = 0.82, 95% CI: 0.75, 0.90) and a similar reduction in dementia risk (RR = 0.82, 95% CI: 0.73, 0.93) compared to those with the lowest intake.
For Alzheimer’s disease specifically, the risk was 20% lower among high consumers (RR = 0.80, 95% CI: 0.67, 0.96). The protective effect appears to follow a dose-response pattern, with the greatest benefit observed up to 150 grams of fish per day, which was associated with a 30% reduced risk of cognitive impairment/decline (RR = 0.70, 95% CI: 0.52, 0.95)
The fattier the fish, the better it is for your brain, with fatty fish rich in omega-3 fatty acids, such as salmon, sardines, mackerel, and tuna, being particularly beneficial due to their high content of docosahexaenoic acid (DHA), a key component for brain health and memory function.
A research study entitled, Fish consumption and omega-3 fatty acid supplementation for prevention or treatment of cognitive decline, dementia or Alzheimer’s disease in older adults - any news?, concluded the following:
The accumulated knowledge indicates that healthy populations may have preventive benefits from fish and docosahexaenoic acid intake, like older adults with memory complaints/mild cognitive impairment, and maybe subgroups of patients with mild/moderate Alzheimer’s disease may also show such benefits. Still, more studies are needed.
In conclusion, it is vital to optimize the diet in order for the low dose lithium orotate, Ivermectin, Fenbendazole and nutraceuticals to be as efficacious as possible; in other words, to reverse dementia Alzheimer’s the diet may very well be nearly as important as the various supplements and repurposed compounds.
And, of course, staying away from any and all vaccines so as to prevent brain damage is critical.
Do NOT comply.






Typos (mostly) edited.
Apologies.
Thank you for speaking truth about the bioweapon vaccines. Slowly people are waking up to the truth, and information is key to helping people to know the truth from the decades of psychological programming.